Patient Background
This is a 66-year-old woman who presented with symptoms of IBS-D, persistent bloating, and abdominal discomfort after meals. She got a recent diagnosis of hydrogen-dominant SIBO confirmed by Trio-Smart breath testing.
Her symptoms began following an episode of food poisoning in the summer of 2025, after which she developed increased food sensitivity and postprandial bloating. Along with periodic loose stools, she continued to struggle with intolerance to certain vegetables and abdominal discomfort.
She had been evaluated by a gastroenterologist and prescribed ciprofloxacin for her SIBO, which she elected not to take. Instead, she started a low-FODMAP diet, which led to partial symptom improvement.
Symptom Profile
At presentation, her primary symptoms included:
- Postprandial abdominal discomfort
- Bloating, particularly after certain vegetables
- IBS-D
- Food sensitivities despite generally healthy eating
She noted improvement after reducing high-fermentation foods, including cruciferous vegetables. She had recently found Dr. Rajsree’s educational content and had independently begun Phase 1 of the SIBO Protocol prior to her initial visit.
Past Medical History
- Hyperlipidemia
- Overactive bladder
She had been prescribed trospium chloride, an anticholinergic medication, for overactive bladder. However, she reported minimal benefit and continued to wake up as many as five times nightly to urinate.
Diet and Lifestyle
- Generally follows a paleo-style diet, focused on whole foods
- Regular physical activity including walking and Pilates
- Did enjoy caramel chews from Trader Joe’s
Her weight had increased from 132 lbs to 142 lbs gradually, despite persistent digestive symptoms.
Prior Diagnostic Workup
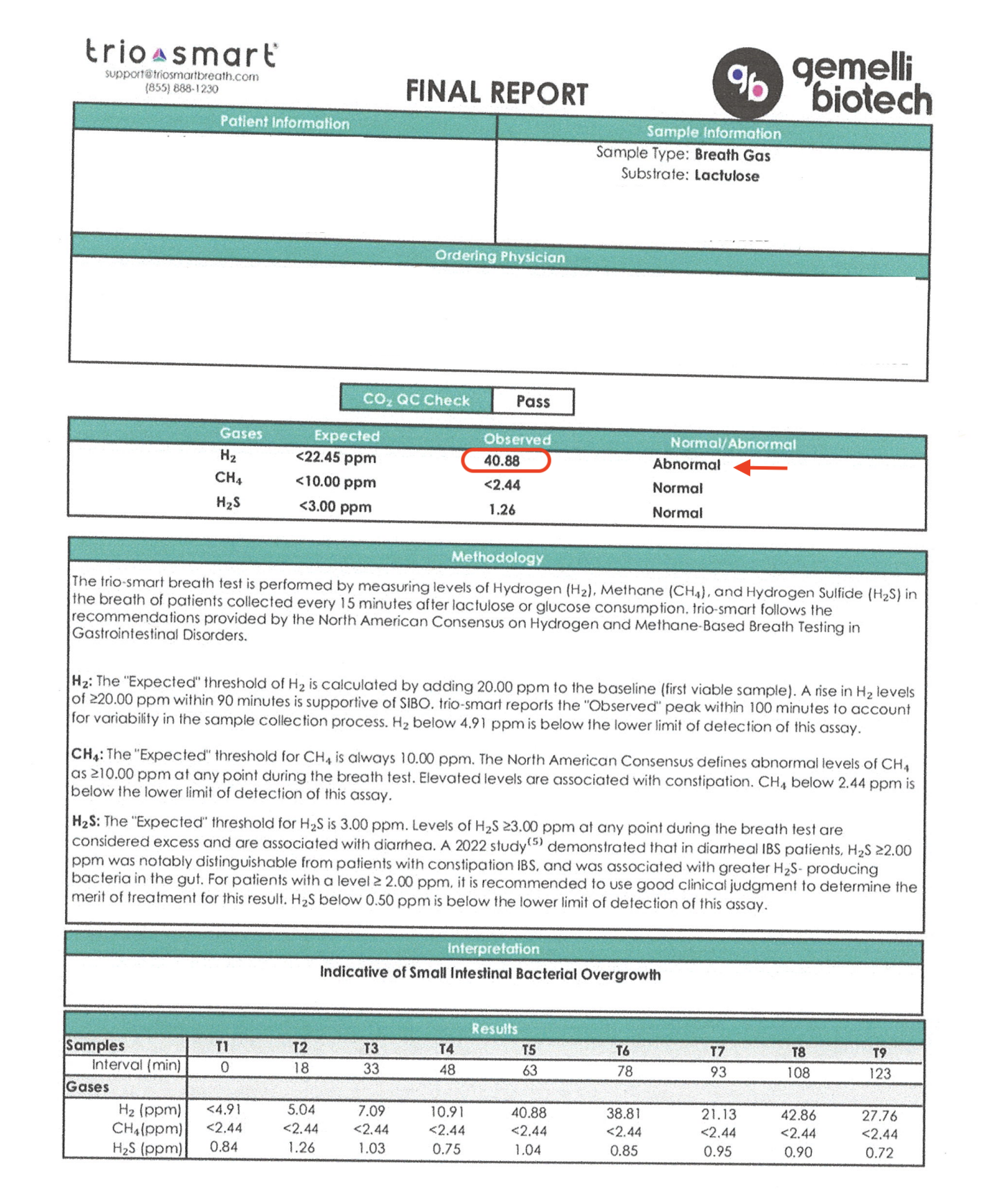
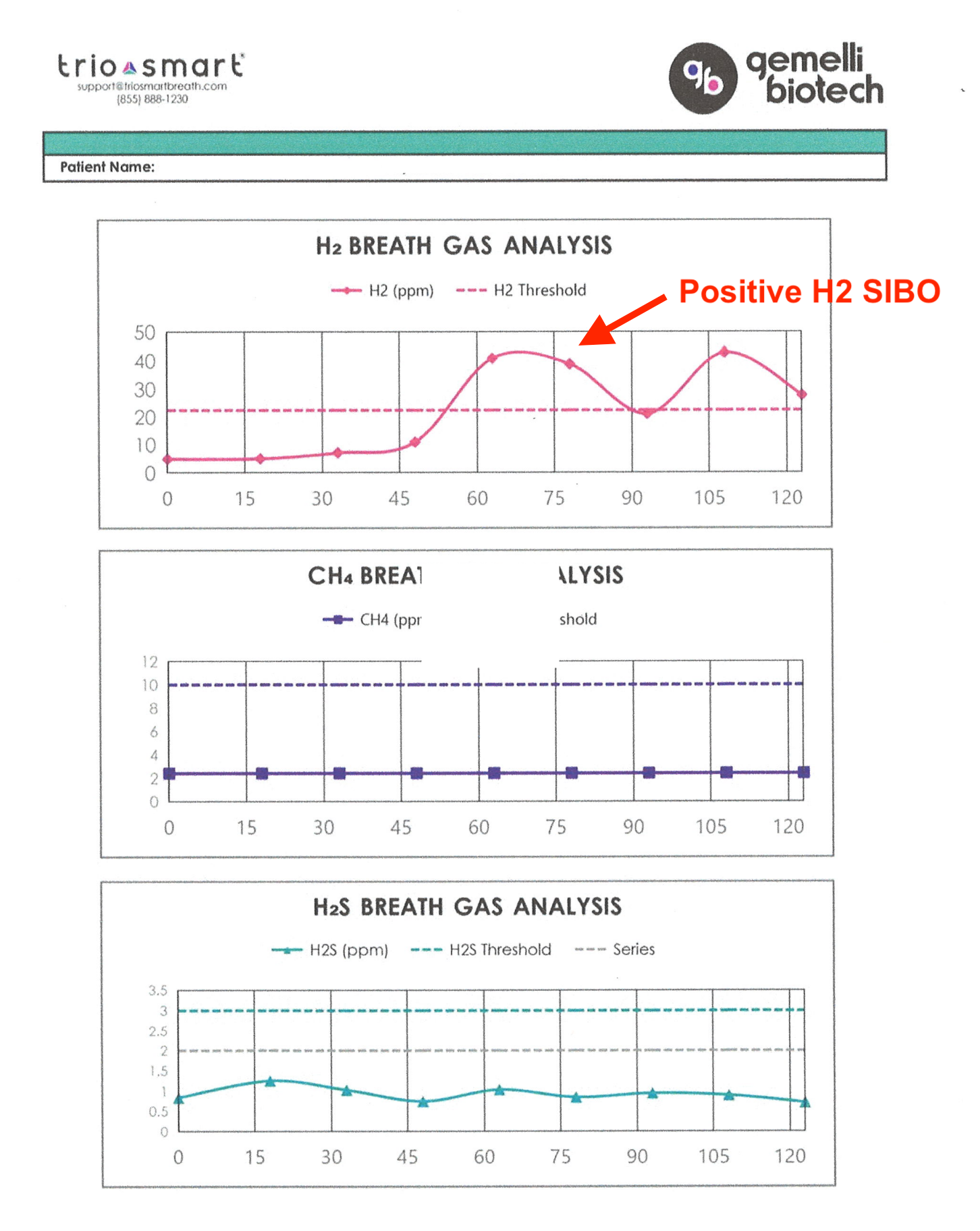
- Trio-Smart SIBO breath test:
- Hydrogen (H₂): 41 ppm — positive for hydrogen-dominant SIBO


- Gastric emptying study (8/2025): Normal
- Esophagram (7/2025): Small hiatal hernia
- EGD and colonoscopy (2025): No significant abnormalities
On physical examination, her abdomen was non-distended with no tenderness to palpation.
Treatment: Dr. Rajsree’s 4-Phase SIBO Protocol
She proceeded with Dr. Rajsree’s structured SIBO protocol, focusing on motility support, digestive support, and targeted herbal antimicrobials. Total antimicrobial treatment duration was 6 weeks.
She was advised to stop trospium chloride, the anticholinergic medication for her bladder as it was not improving her bladder symptoms and may be potentially impacting gut motility.
Phase 1–2: Promoting Motility and Supporting Digestion
- Digestive Enzyme Pro – 1–2 capsules after every meal
- Essential Magnesium – 2 capsules at bedtime
- Motility Activator – 1 capsule at bedtime
Phase 3–4: Reduce Inflammation and Targeted Antimicrobial Therapy
Next, the following were added:
Spore Probiotic IgG – 3 capsules daily in the morning on an empty stomach
Berberine Pro – 1 capsule after every meal for 6 weeks
Oregano Oil – 1 capsule after every meal for 6 weeks
Dietary Strategy:
She followed the low FODMAP / low lectin SIBO diet, with specific instructions to practice meal spacing:
- Avoid snacking between meals
- Maintain 4–5 hours between meals
- Maintain a 12-hour overnight fast between dinner and breakfast
- Intermittent fasting — encouraged to support migrating motor complex (MMC) activity
Outcomes
After completing 6 weeks of the herbal antimicrobial phase, repeat Trio-Smart breath testing showed:
- Hydrogen (H₂): decreased from 41 ppm → 25 ppm, now within the normal range (≤26 ppm on Trio-Smart)


Clinically, she experienced:
- Complete resolution of IBS-D symptoms
- Marked improvement in bloating and postprandial discomfort
- Improved tolerance of vegetables and meals
- Continued regular, daily bowel movements
She noted that Digestive Enzyme Pro was particularly helpful and continued to use one capsule after meals, especially during heavier meals such as Thanksgiving, with excellent tolerance.
Maintenance Plan
Following successful treatment, she transitioned into the Prevention of Relapse phase:
- Switched to Probiotic 100 Billion for microbiome rebuilding for 1 month
- After 1 month, she transitioned to an alternating maintenance probiotic strategy:
- Probiotic 20 Billion with Saccharomyces boulardii
- Probiotic 20 Billion with Lactobacillus reuteri
She continued:
- Digestive Enzyme Pro with meals
- Essential Magnesium (2 capsules at bedtime)
- Motility Activator (1 capsule at bedtime or in the morning on an empty stomach)
Key Insights
This case highlights a classic presentation of post-infectious hydrogen-dominant SIBO following food poisoning, causing IBS-D.
Contributing factors likely included:
- Post-infectious motility impairment
- Ongoing anticholinergic medication use, which can further slow gut motility
- Dietary fermentation triggers despite generally healthy eating
Importantly, this patient achieved objective normalization of breath testing and full resolution of IBS-D symptoms using a structured, non-pharmaceutical, herbal-based SIBO protocol.