Patient Background
This is the case of a 69-year-old woman who presented with persistent bloating and periodica sharp pain in the left upper abdomen. Her medical history was significant for hypothyroidism, food sensitivities, lactose intolerance, prior cholecystectomy (gallbladder removal), and previous pelvic surgeries involving a bladder sling and mesh. She also had a prior 15-year history of proton pump inhibitor (PPI) use, a stomach-acid suppressive medication, which she strongly believed contributed to her digestive issues. Following her cholecystectomy, she struggled with digestion and progressively developed more restrictive eating habits to control her symptoms, leading to an unintended weight loss from 137 lbs to 114 lbs. Family history was notable for a daughter with Celiac disease.
Prior Treatment Challenges
A CT scan of the abdomen and pelvis was unremarkable. Despite ongoing symptoms, her prior physician prescribed two rounds of Rifaximin and Neomycin without confirming a diagnosis of SIBO through breath testing. These treatments provided no relief and worsened her brain fog.
Her bowel movements were soft and formed but characteristically thin, with a tendency toward constipation.
On examination, her abdomen was mildly distended with tenderness to palpation in the lower abdomen.
SIBO Breath Testing
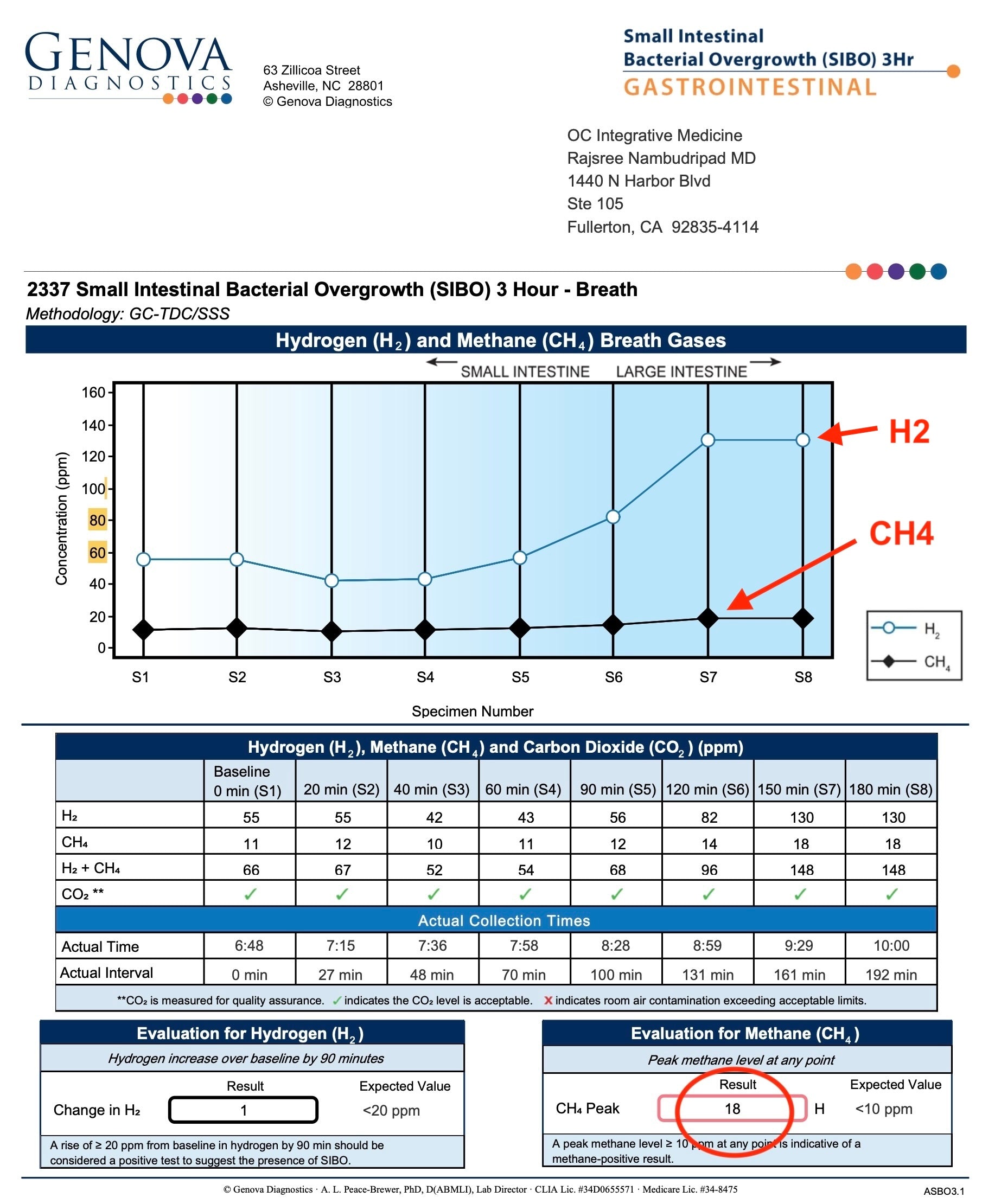
Comprehensive lactulose breath testing revealed:
- Methane (CH₄) level: 18 ppm — positive for Intestinal Methanogen Overgrowth (IMO)
- Hydrogen (H₂) level: 55 ppm at baseline, rising to 82 ppm at 120 minutes (up to 120 minutes can be the small intestine). While the elevated baseline hydrogen suggested a possible issue with test preparation, the rise during the first 120 minutes still indicated active small intestinal bacterial overgrowth.

Additional labs confirmed:
- Negative tissue transglutaminase (TTG IgA), ruling out Celiac disease
- Negative IgE-mediated food allergies
Treatment: Implementing Dr. Rajsree’s 4 Phase SIBO Herbal Protocol
Phase 1-2: Promoting Motility and Reducing Gas Levels:
She was started on:
- Essential Magnesium (4 capsules at bedtime)
- Motility Activator (at bedtime)
- Digestive Enzyme Pro (2 capsules after meals)
- Betaine and Pepsin (1 capsule after meals)
- Aloe Pro (as needed for constipation)
Dietary Strategy:
She began a low FODMAP / low lectin SIBO diet, with specific instructions to practice meal spacing:
- Avoid snacking between meals.
- Maintain 4–5 hours between meals.
- Maintain a 12-hour overnight fast between dinner and breakfast.
She was quite strict in following the recommended diet consuming low-fermentation foods including basmati rice, carrots, spinach, and chicken.
Within weeks, she experienced remarkable improvements in bowel regularity, bloating, and resolution of left upper quadrant pain — even before initiating antimicrobial therapy.
Phase 3-4: Reduce Inflammation and Targeted Antimicrobial Therapy
In the next phases of the protocol, we introduced Spore Probiotics and targeted herbal antimicrobials to address bacterial and methanogen overgrowth:
Addition of:
- Spore Probiotic IgG (3 capsules daily in AM on empty stomach).
- Berberine Pro 1 capsule after each meal.
- Oregano Oil 1 capsule after each meal.
- Atrantil (2 capsules after each meal; substituted for Allicidin due to garlic sensitivity).
Outcomes
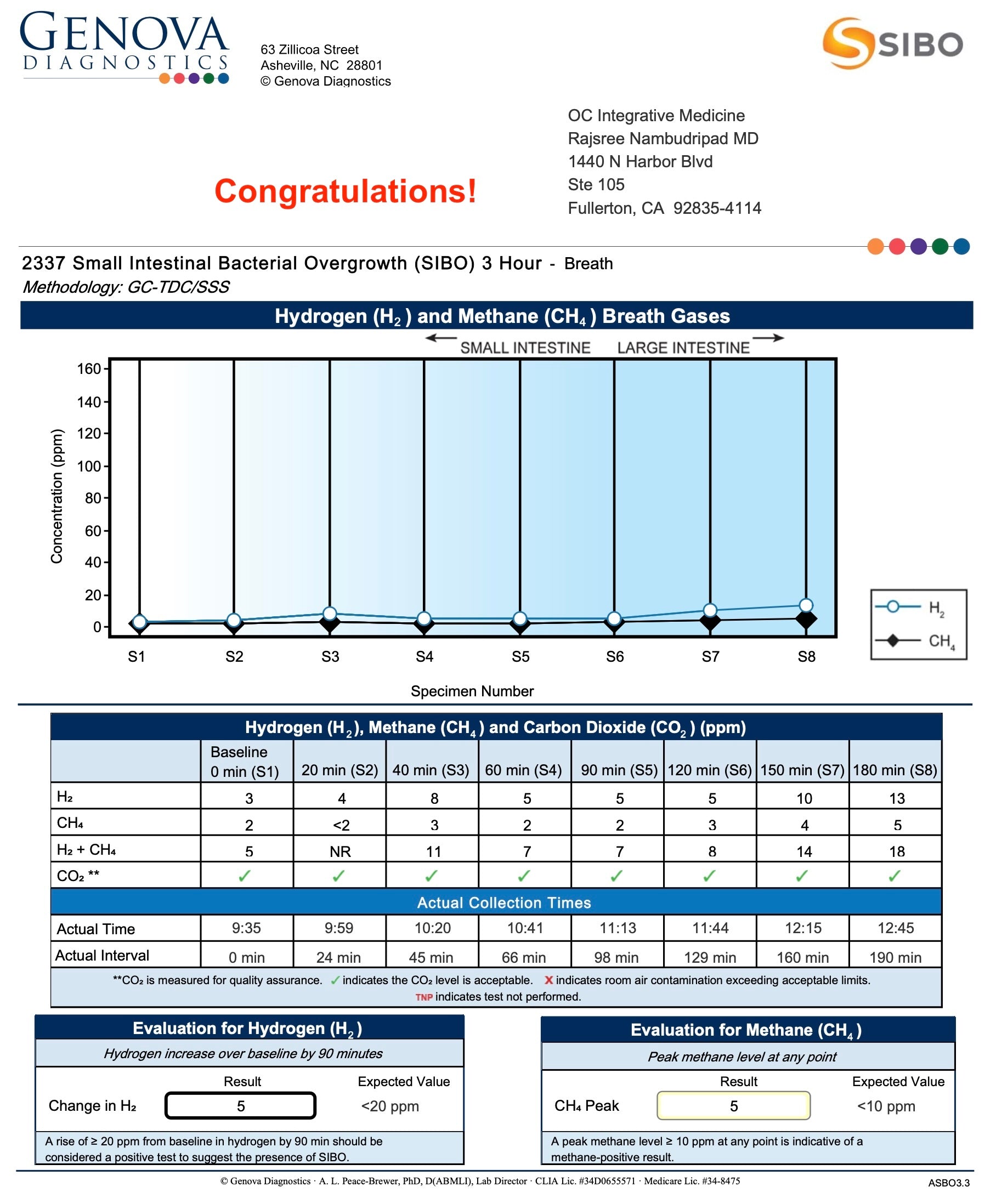
After six weeks herbal antimicrobials, her repeat SIBO breath test showed:
- Methane (CH₄): decreased from 18 ppm → 5 ppm (normalized)
- Hydrogen (H₂): decreased from 82 ppm → 5 ppm

Clinically, she achieved full resolution of her symptoms: normalization of bowel habits, complete resolution of bloating and abdominal pain, stabilization of weight, and significant improvement in energy. Her sinus symptoms improved as well!
Maintenance Plan
- She transitioned into the "Prevention of Relapse” phase of Dr. Rajsree’s SIBO Protocol, also focusing on microbiome restoration.
- She was transitioned to Probiotic 100 Billion (a broad-spectrum probiotic for microbiome rebuilding)
- Continuation of Essential Magnesium, Motility Activator, Digestive Enzyme Pro, and Betaine and Pepsin
- Gradual tapering off of Aloe Pro, a stimulant laxative, or using just as needed
Key Insights
This case illustrates how Intestinal Methanogen Overgrowth (IMO) can present in complex, multifactorial cases involving:
- Long-term PPI use (15 years), which shuts off stomach acid production, allowing bacteria to grow in the small intestine
- Changes in digestion after gallbladder removal, commonly seen due to impaired fat absorption
- Restrictive dieting to control symptoms, leading to unintended weight loss
- A background of thyroid dysfunction, food sensitivities, and prior pelvic surgeries affecting motility
Despite multiple unsuccessful rounds of pharmaceutical antibiotics (Xifaximin + Neomycin) without breath testing, this patient responded beautifully to Dr. Rajsree’s 4-Phase SIBO Herbal Protocol. Her case underscores the importance of:
- Proper diagnosis through breath testing
- Sequential treatment beginning with digestive and motility support
- Use of well-tolerated herbal antimicrobials, even in sensitive patients
Treatment led to normalization of her SIBO breath test, resolution of bloating and abdominal pain, regular bowel movements, improved digestion, and stabilization of her weight — all without reliance on pharmaceuticals.
This case also emphasizes how non-gastrointestinal symptoms (such as brain fog and sinus issues) may improve when the root cause in the gut is addressed.
Patient Testimonial:
"It was Christmas Eve and I was stuck in the bathroom! I had taken the second round of the popular antibiotics for SIBO/IBS, and my gut was too weak to tolerate them. At my lowest point I turned the TV on, and on YOUTUBE were videos of Dr. Rajsree talking about the gut and SIBO/IBS. She was describing all of my symptoms! January 10, I met with Dr. Rajsree in person. She gave me a plan with diet, natural medicine, and herbal medicinals instead of the antibiotics. It really worked! I am whole! Dr. Rajsree laughs when I say, 'You saved my gut; you saved my life!'"