Patient Background
This is the case of a 43-year-old Indian American man who presented with chronic bloating, abdominal discomfort, and a history of recurrent SIBO. His past medical history was notable for fatty liver disease.
He first experienced symptoms in 2021 after drinking aloe vera juice daily for a month, which triggered new bloating and gas. An initial consultation with a gastroenterologist led to a trial of a low FODMAP diet for one month, but this provided no relief. He underwent an endoscopy or colonoscopy, as well as an abdominal ultrasound, both of which were reportedly unremarkable. He was empirically prescribed the antibiotic Xifaxan without SIBO testing, which successfully resolved his symptoms.
However, two months later, his symptoms returned. Another course of Xifaxan provided temporary relief, but over time, he developed dietary sensitivities, notably to gluten (eliminated 7–8 years ago), dairy (eliminated in 2021), certain fruits (such as mango), eggs, goat meat, and cucumbers — all of which triggered bloating and discomfort.
He found some symptom relief by self-initiating Betaine HCl with meals and TUDCA at bedtime. His bowel movements were daily but sometimes incomplete. Four weeks prior to our consultation, he experienced a new flare characterized by an "empty" feeling in the stomach even after eating, accompanied by weakness and persistent hunger. An urgent care visit with CT scan and H. pylori testing yielded negative results. His primary care physician prescribed another course of Xifaxan, which temporarily improved his symptoms, but within two weeks, bloating and abdominal discomfort recurred.
By the time he had consulted me, he had already done 3 prior courses of the antibiotic Xifaxan!
Diet history included:
- Breakfast: gluten-free toast with peanut butter or a gluten-free cereal bar.
- Lunch and dinner: chicken, rice, and some vegetables prepared with Indian spices.
The initial consultation was conducted via video visit, during which abdominal distension was noted.
Treatment: Implementing Dr. Rajsree’s 4-Phase SIBO Protocol
Phase 1-2: Promote Motility and Reduce Gas Levels '
He was started on:
- Digestive Enzyme Pro (1–2 capsules after each meal)
- Betaine and Pepsin (1–2 capsules after each meal)
- Essential Magnesium (2–4 capsules at bedtime, adjusted to bowel tolerance)
- Motility Activator (1–2 capsules at bedtime)
Dietary Strategy:
He began a low FODMAP / low lectin SIBO diet, with specific instructions to practice meal spacing:
- Avoid snacking between meals
- Maintain 4–5 hours between meals
- Maintain a 12-hour overnight fast between dinner and breakfast
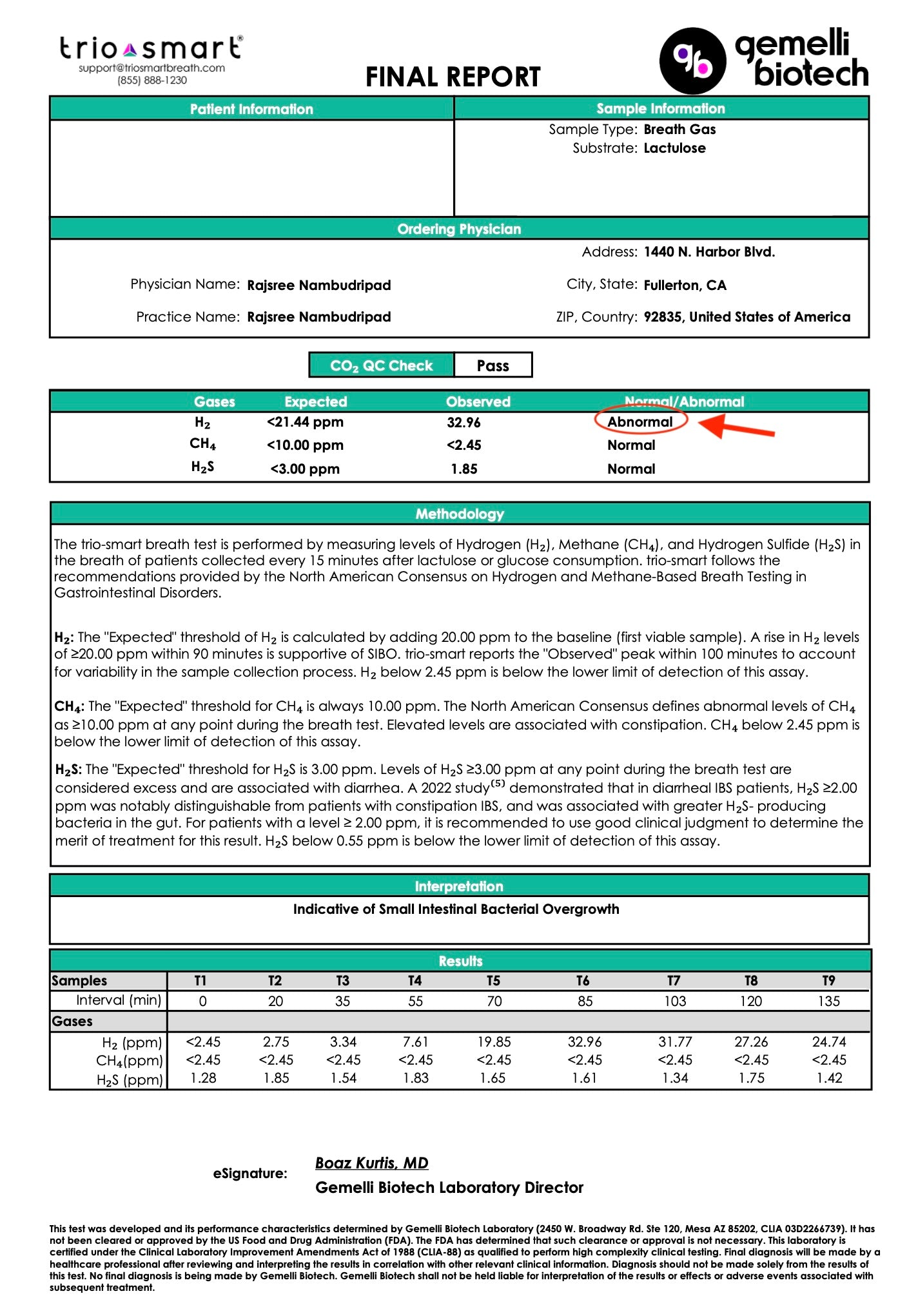
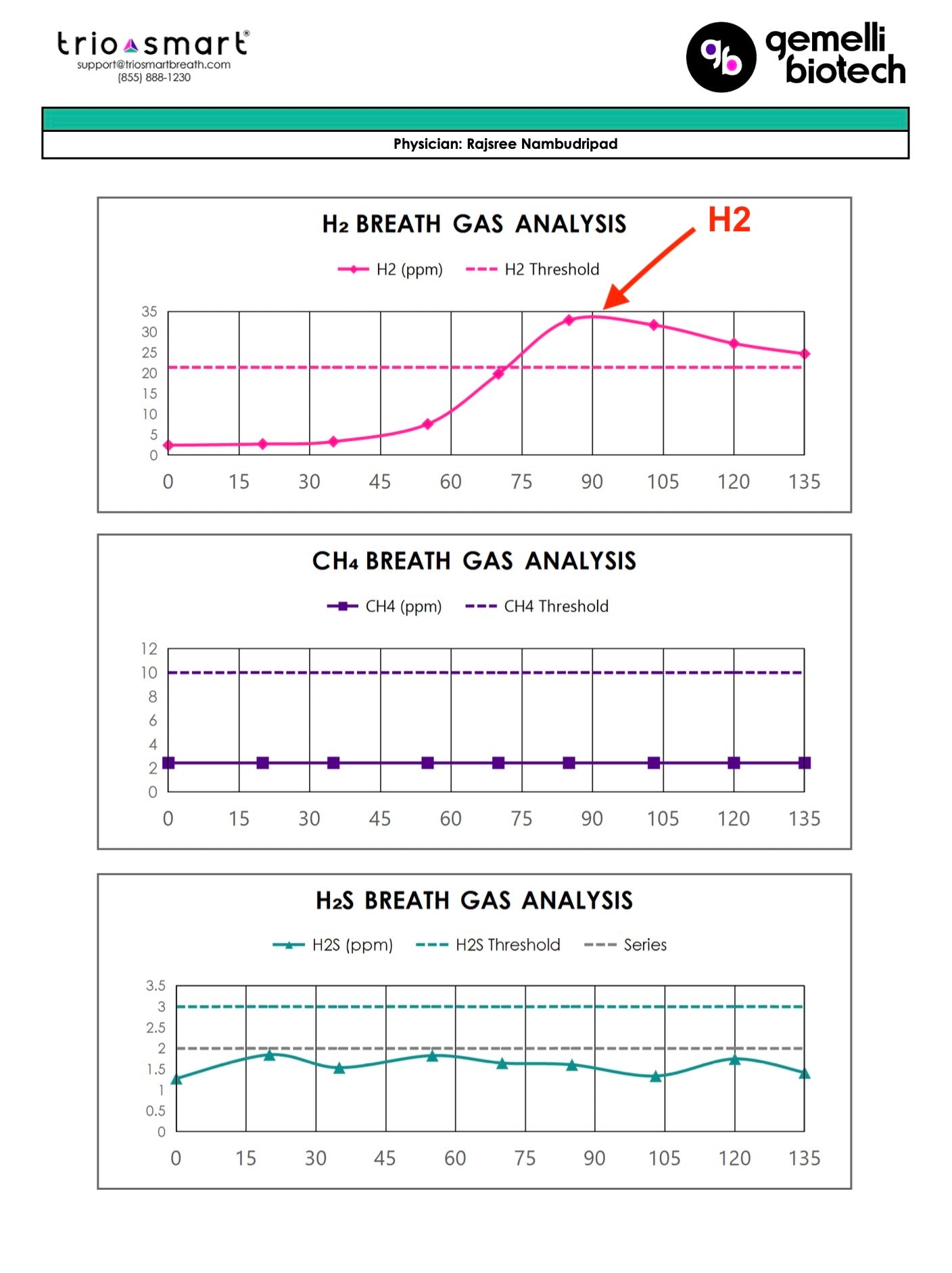
SIBO Breath Testing
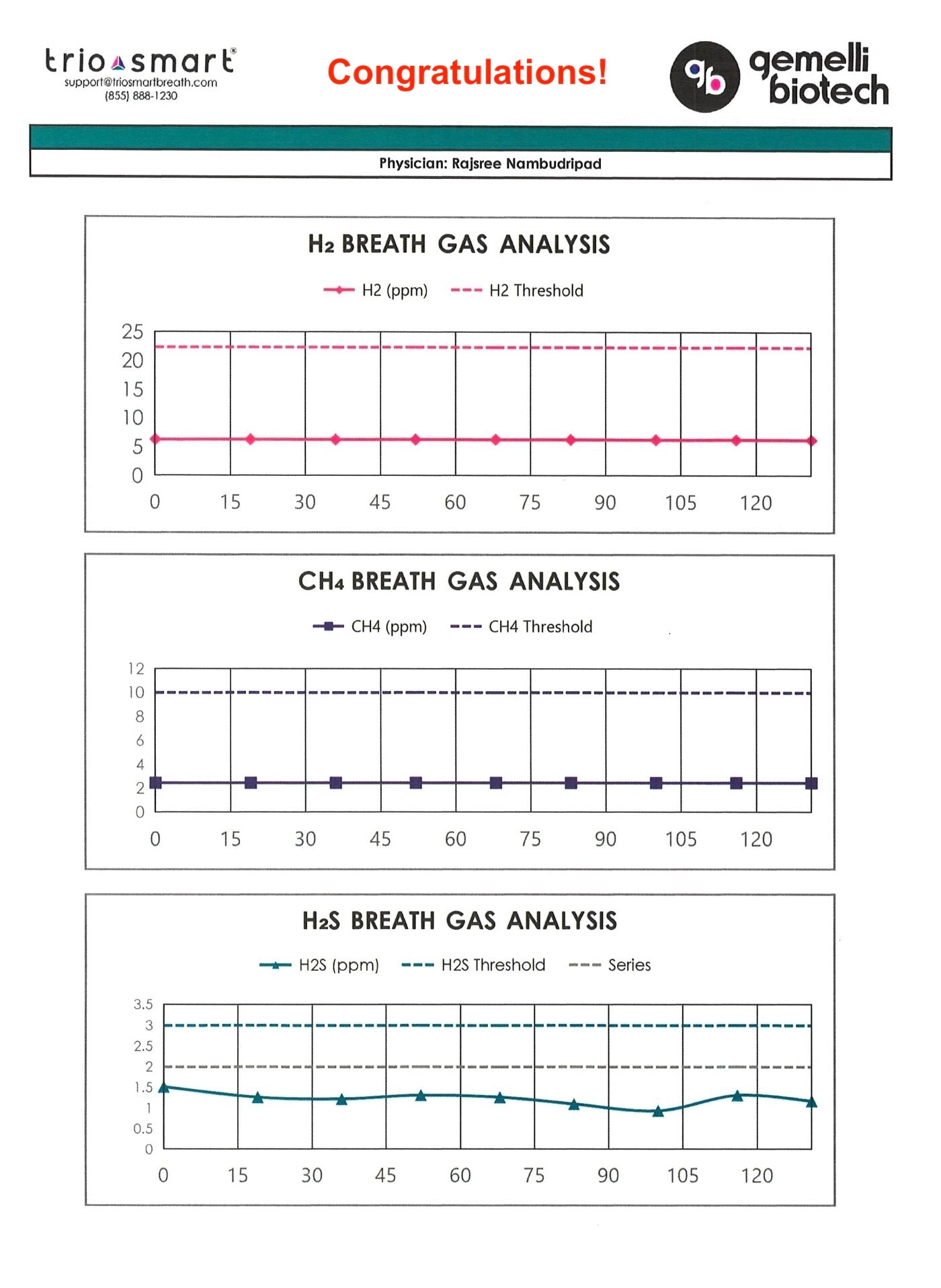
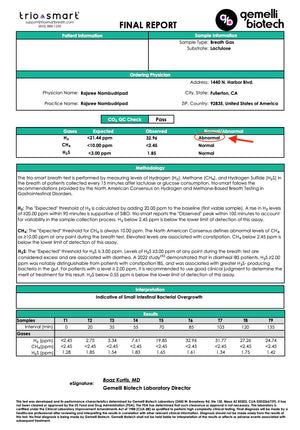
Initial lactulose breath testing revealed:
- Hydrogen (H₂) level: 32.96 ppm — diagnostic for hydrogen-dominant SIBO


Additional testing included an IgE food allergy panel, which was negative, helping to exclude true food allergies as the cause of symptoms.
Phase 3-4: Reduce Inflammation and Targeted Antimicrobial Therapy
In the next phases of the protocol, we introduced Spore Probiotics and targeted herbal antimicrobials to address bacterial overgrowth:
Addition of:
- Spore Probiotic IgG (3 capsules in the morning on an empty stomach)
- Berberine Pro (1 capsule after each meal) for 6 weeks
- Oregano Oil (1 capsule after each meal) for 6 weeks
Outcomes
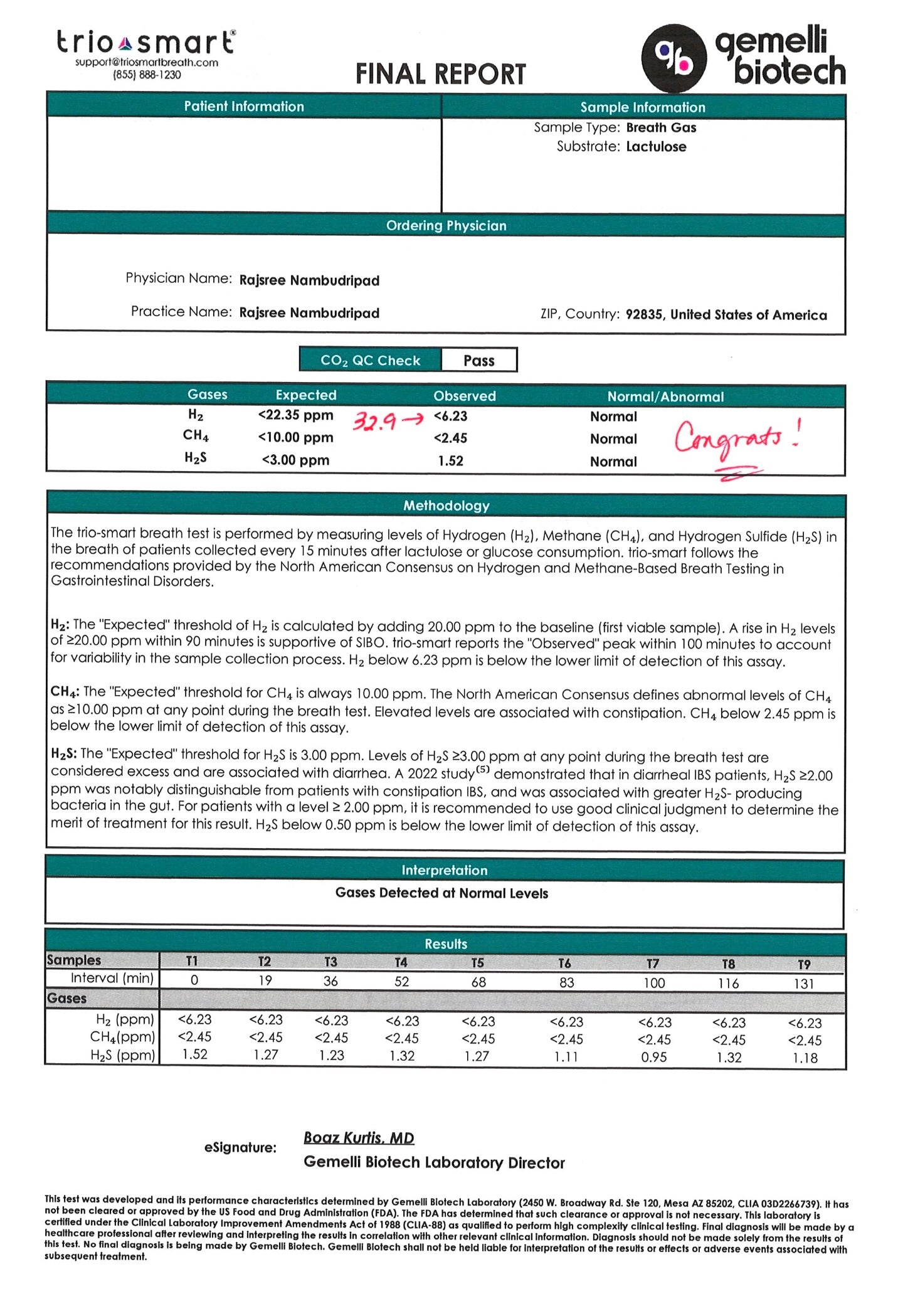
Upon completion of the antimicrobial phase, repeat SIBO breath testing revealed:
Hydrogen (H₂): < 6 ppm — complete eradication of SIBO

 Clinically, he experienced:
Clinically, he experienced:
- Resolution of bloating and abdominal discomfort
- Regular, complete bowel movements
- An 8-pound weight loss, which he welcomed
- He also successfully began reintroducing previously restricted foods without significant symptom recurrence.
Maintenance Plan
To prevent relapse, we transitioned him to the “Prevention of Relapse” Phase:
- Transitioned to Probiotic 100 Billion (broad-spectrum microbiome support)
- Continued Digestive Enzyme Pro and Betaine and Pepsin with meals
- Continued Essential Magnesium and Motility Activator at bedtime
He was advised that now that his SIBO was resolved, if any lingering symptoms developed, a comprehensive stool microbiome profile could be considered to evaluate further gut health. At the time of writing, he has not needed any additional follow-up, suggesting continued success and stability.
Key Insights
This case demonstrates how repeated rounds of antibiotics (Xifaxan)—even when temporarily effective—often fail to produce lasting results when the underlying causes of SIBO are not addressed. This patient relapsed multiple times after taking Xifaxan, never having completed a formal breath test or addressing the deeper issues driving his symptoms.
It wasn’t until he followed Dr. Rajsree’s 4-Phase SIBO Protocol that he achieved sustained improvement.
What made the difference:
- Motility support with Motility Activator, a prokinetic, addressing sluggish transit and preventing bacterial buildup.
- Digestive support with Digestive Enzyme Pro and Betaine and Pepsin, improving breakdown and absorption of nutrients.
- Phased herbal antimicrobials to gently and effectively reduce bacterial overgrowth.
- A structured SIBO diet with meal spacing to support the migrating motor complex (MMC) to allow time for proper small intestine cleaning.
Together, these interventions led to complete resolution of SIBO on breath testing, normalized bowel movements, and long-term digestive stability.
This case is a powerful example of how Dr. Rajsree’s SIBO Protocol addresses not just bacterial overgrowth—but the underlying root causes that cause it to persist and recur, resulting in lasting results.
Patient Testimonial:
"I am very grateful to have found Dr Rajsree. I was dealing with gut issues for a while and even with multiple visits over the years to a gastroenterologist only relieved my symptoms temporarily. It has been 5 months I started Dr Rajsree's treatment and so far it has been great. And I hope it stays that way. She is also very polite and easy to talk to. Again very thankful to have found a Dr who has deep understanding of underlying issues."